In the late 1900s, psychologists and neuroscientists noted a link between drugs that affected dopamine pathways in the brain and symptoms associated with schizophrenia. This led to a theory of what may cause the complex disease of schizophrenia and how we could work to treat it more effectively.
Schizophrenia is a complex mental disorder with symptoms that include delusions, hallucinations, disorganized speech, and disorganized behavior. Over the years, several theories have emerged in an attempt to unravel the intricate nature of schizophrenia. However, one hypothesis that has gained considerable attention and has significant research backing it is the dopamine hypothesis.
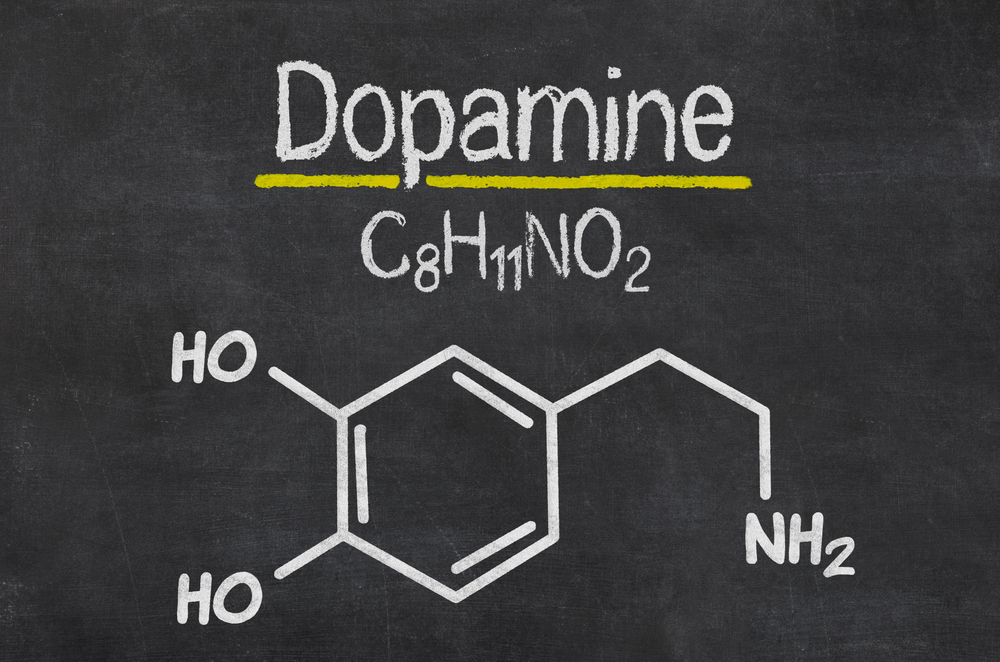
The idea behind this hypothesis is that when it comes to schizophrenia, there’s a problem with the balance or regulation of dopamine in a person’s system. Dopamine is a chemical messenger in the brain that helps with various functions, such as motivation, pleasure, and energy. This hypothesis has not only given us valuable insights into how the disorder works in the brain, but has also influenced the development of antipsychotic medications that specifically target dopamine receptors.
Recommended Video for you:
Study of Involvement of Dopamine in Schizophrenia
For years, scientists have been puzzled about what causes schizophrenia. Is it caused by genetics, a chemical imbalance in the brain, or environmental conditions and traumatic experiences? Though we don’t have a conclusive answer to this question, a lot of research on schizophrenia has implicated dopamine as a significant factor. This understanding comes from three major pieces of evidence (observations).
In 1952, a French surgeon named Henri Laborit discovered a drug called chlorpromazine (Thorazine), which reduced hallucinations and delusions in schizophrenic patients. The drug works by blocking dopamine receptors in the brain, consequently reducing dopamine’s effects in the brain.
The second piece of evidence came from the discovery that amphetamines cause psychosis. Amphetamines increases dopamine in the brain. This leads to over-stimulation of the brain to the available dopamine, which induces schizophrenia-like symptoms. For instance, a study found that consistent use of LSD can lead to paranoid-schizophrenia-like symptoms.
The third observation comes from studying Parkinson’s disease, which is caused by low levels of dopamine. It was observed that when Parkinson’s patients were given a drug known as L-DOPA, which increases dopamine receptors in the brain, it led to patients experiencing schizophrenia-like symptoms.
All of this circumstantial evidence points toward the role of dopamine in inducing schizophrenia-like symptoms.

How does dopamine affect schizophrenia?
The activity of the dopaminergic system can influence how much attention a person pays to both internal and external events. Disregulated dopamine transmission can lead to individuals paying more attention to and attaching more importance to stimuli that are not relevant. This is referred to as “aberrant salience.”
This helps explain why people may develop delusions or experience hallucinations, as they almost always report high levels of sensory awareness (e.g., “My senses were heightened” or “I developed a fascination with the seemingly insignificant details around me”), or they report an increased significance of the events around them (“I felt that this situation had an overwhelming importance”).
These individuals struggle to make sense of experiences that had previously existed in the background, but have now (seemingly) become extremely important. For example, they may perceive the white noise hum of a refrigerator as a voice speaking to them, or they may think that a package arriving at an inopportune time is a viable threat.
The functional excess of dopamine occurs when there is a lot of dopamine available in the synapse. This can happen through an increase in synthesis (less absorption of dopamine), an increase in the production of dopamine, when the brain releases too much dopamine in the synapse directly, or the slowing down of the rate at which dopamine is broken down once it is in the synapse. It can also occur if there is a blockage in the neuronal re-uptake of dopamine. As mentioned before, sometimes the receptors on which the dopamine acts is either very dense or very sensitive, which makes the brain react as if there is too much dopamine in the brain, when only a normal amount of it is actually present.
Is Dopamine the only neurotransmitter involved in schizophrenia?
No. Schizophrenia is a complex disease and a single neurotransmitter isn’t the exclusive cause. New research findings have also implicated the involvement of glutamate, which is a key excitatory neurotransmitter. This evidence comes from the observation that phencyclidine (PCP or angel dust), a drug that blocks glutamate receptors, causes schizophrenia-like symptoms in people. Moreover, when people diagnosed with schizophrenia take PCP, their symptoms seem to worsen.
People with schizophrenia have low levels of glutamate in their brain. Neurocognitive researchers Olney and Farber proposed that there are lower levels of activity of several types of glutamate receptors (NMDA receptors) in people who have schizophrenia. This can result in the loss of neurons in critical brain regions and cause symptoms resembling schizophrenia. Subtle brain injury may happen if the NMDA receptors aren’t ordinarily activated (possibly because glutamate levels are low).
All in all, this glutamate hypothesis, along with the dopamine hypothesis, is gaining traction in the research area of schizophrenia. Both hypotheses are promising and are leading to the development of newer drugs that can provide better means of treatment for countless people around the world.
References (click to expand)
- KA Hewitt. (2002) LSD and changing ideas of mental illness, 1943–1966. search.proquest.com
- Kunz, E. (2014, March 31). Henri Laborit and the inhibition of action. Dialogues in Clinical Neuroscience. Informa UK Limited.
- Rognli, E. B., & Bramness, J. G. (2015, September 28). Understanding the Relationship Between Amphetamines and Psychosis. Current Addiction Reports. Springer Science and Business Media LLC.
- Nieoullon, A. (2002, May). Dopamine and the regulation of cognition and attention. Progress in Neurobiology. Elsevier BV.
- Seeman, P. (1987). Dopamine receptors and the dopamine hypothesis of schizophrenia. Synapse. Wiley.
- Vincent, J. P., Kartalovski, B., Geneste, P., Kamenka, J. M., & Lazdunski, M. (1979, September). Interaction of phencyclidine ("angel dust") with a specific receptor in rat brain membranes. Proceedings of the National Academy of Sciences. Proceedings of the National Academy of Sciences.
- Uno, Y., & Coyle, J. T. (2019, March 6). Glutamate hypothesis in schizophrenia. Psychiatry and Clinical Neurosciences. Wiley.
- Olney, J. W. (1995, December 1). Glutamate Receptor Dysfunction and Schizophrenia. Archives of General Psychiatry. American Medical Association (AMA).
- Hu, W., MacDonald, M. L., Elswick, D. E., & Sweet, R. A. (2014, October 14). The glutamate hypothesis of schizophrenia: evidence from human brain tissue studies. Annals of the New York Academy of Sciences. Wiley.
- LSD Statistics - LSD, Mushrooms, Mescaline & Other .... Foundation for a Drug-Free World
- Fuentes, J. J., Fonseca, F., Elices, M., Farré, M., & Torrens, M. (2020, January 21). Therapeutic Use of LSD in Psychiatry: A Systematic Review of Randomized-Controlled Clinical Trials. Frontiers in Psychiatry. Frontiers Media SA.
- Vardy, M. M. (1983, August 1). LSD Psychosis or LSD-Induced Schizophrenia?. Archives of General Psychiatry. American Medical Association (AMA).
- Mahmood, D., Alenezi, S. K., Anwar, M. J., Azam, F., Qureshi, K. A., & Jaremko, M. (2022, May 23). New Paradigms of Old Psychedelics in Schizophrenia. Pharmaceuticals. MDPI AG.
- Krebs, T. S., & Johansen, P.-Ø. (2013, August 19). Psychedelics and Mental Health: A Population Study. (L. Lu, Ed.), PLoS ONE. Public Library of Science (PLoS).