Table of Contents (click to expand)
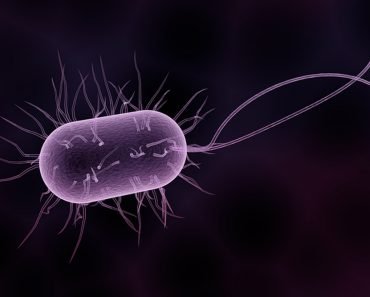
Bacteria that have acquired resistance to antibiotics, also known as superbugs, are a serious concern for healthcare. They’re a product of overusing antibiotics, not only in humans, but also for livestock; the more that the bacteria is exposed to the antibiotic, the higher its chances are of evolving resistance.
Bacteria are everywhere, from your phone screen to the 400°C hydrothermal vents on the ocean floor. We house some “good ones” in and on our bodies, which help keep our gut and skin healthy, but many bacteria can make you sick.
Since Alexander Fleming discovered penicillin in 1928, antibiotics have been a super solution to bacterial infections. Antibiotics kill bacteria, but by random chance (aka evolution), a bacteria may manage to resist the killing effect of the antibiotic. If that antibiotic-resistant bacteria reproduces, it will pass on that resistance to its offspring.
According to the reports of 2019, each year, around 2.8 million multiple drug-resistant ailments occur in the United States alone, leading to more than 35,000 annual fatalities.
Recommended Video for you:
Where Do We Use Antibiotics And How Does It Affect Us?
Antibiotics have revolutionized the public health sector. Their use meant that people needn’t die from diseases such as cholera, typhoid, pneumonia or syphilis. For instance, in the US, since the surge of antibiotics, non-communicable diseases replaced communicable diseases as the leading cause of death, and the average life expectancy at birth has increased to 78.8 years.
Today, antibiotics are an indispensable part of our medical system, but we’re also overusing them.
Overconsumption By Humans
Research shows that microbial resistance to drugs is higher in countries with higher antibiotic usage and an overprescription problem.
Antibiotic use grew by 46% between 2000 and 2018, according to one study. Within those years, developing nations saw the biggest jump in antibiotic use, specifically, a 76% increase in low- and middle-income nations. South Asia experienced the biggest spike in antibiotic usage levels… increasing by 116%!
A number of multidrug resistant (MDR) and even extremely drug-resistant (XDR) bacterial pathogens or superbugs have emerged over the past 20 years as a result of the overuse and careless application of clinically prescribed antibiotics.
Antibiotics And Livestock
Antibiotics are also used to keep livestock free of disease.

We’re consuming three times more meat than we used to consume 50 years ago. This is in part due to a larger population, as well as higher incomes. Antibiotics decrease the incidence of illness, but they’re also used to increase the growth of the animals.
Reports highlight that 50-80% of all antibiotics sold in developed countries go to livestock. This is seen as beneficial for those rearing the animals.
Bacteria in livestock can develop resistance and enter the environment either through the waste of the animal or in the flesh of the animal. We eventually eat the animal, or food that might have the bacteria on its surface, and we may encounter such a resistant strain. In this way, bacteria from animals can make the jump to humans, and lead to disease if such exposure becomes frequent.
The Hospital Superbug MRSA
The first major case of antibiotic resistance that came to the notice of the public was the hospital superbug, MRSA.
In hospitals, before antibiotics were developed in the early 1940s, the majority of infections, particularly pneumonia, were caused by Staphylococci aureus.
These bacteria were initially responsive to penicillin, but penicillin-resistant varieties of S. aureus had already appeared by the 1950s. A synthetic penicillin called methicillin was introduced to consumers in early 1960 and was used for the treatment of S. aureus. However, by the end of the 1960s, new methicillin-resistant S. aureus strains had appeared. The strain spread rapidly, and was found around the world by the 1980s.
Methicillin-resistant Staphylococcus aureus (MRSA) became known as the “hospital superbug”. MRSA causes skin infections and other serious effects that can result in pneumonia, bloodstream infections, and even death.
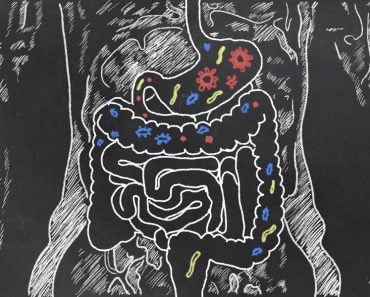
Detrimental Effects On Gut Microbiome
Nearly 40 trillion bacterial and roughly 30 trillion human cells make up the human gut microbiome. The human body’s physiological functions, vitamin production, and immune system are all influenced by the gut microbiome.
Our gut microbiome gets modified when we overconsume broad spectrum antibiotics.
Reduced microbial diversity, modifications to the functional characteristics of the microbiota, and increased susceptibility to pathogenic infection are all antibiotic-induced changes in microbial composition that can have a negative effect on host health. The detrimental effects on human health of rashly taking antibiotics include systemic infections, chronic diarrhea and inflammation.

Conclusion
According to a study published in The Lancet, in 2019, bacterial antimicrobial resistance was linked to approximately 5 million human deaths worldwide. Researchers predict that this will only increase in the coming years.
To tackle this, scientists are looking for solutions. One solution might be bacteriophages—viruses that attack and kill bacteria. Phage treatment would employ bacteriophages that target specific bacteria, such as those linked to infectious diseases.
Most bacteriophages are specific to their targets. While the same does not hold true for antibiotics, many of them target a broad spectrum of bacteria. Doctors and scientists are teaming up and using phage therapy as a last resort for patients who have acquired a multidrug-resistant infection.
Another solution is the “One Health Approach“, which is becoming more popular in the United States and throughout the world as a successful strategy to combat health issues like AMR.
The participating organizations focus on the human, animal, and environmental health sectors and are also accountable for determining the most important areas for action, the best techniques for observing AMR and containing infections, and the laws and regulations that should control the use of antibiotics.
References (click to expand)
- Loc-Carrillo, C., & Abedon, S. T. (2011, March). Pros and cons of phage therapy. Bacteriophage. Informa UK Limited.
- Washer, P., & Joffe, H. (2006, October). The “hospital superbug”: Social representations of MRSA. Social Science & Medicine. Elsevier BV.
- Viana, A. T., Caetano, T., Covas, C., Santos, T., & Mendo, S. (2018, October). Environmental superbugs: The case study of Pedobacter spp. Environmental Pollution. Elsevier BV.
- Browne, A. J., Chipeta, M. G., Haines-Woodhouse, G., Kumaran, E. P. A., Hamadani, B. H. K., Zaraa, S., … Dolecek, C. (2021, December). Global antibiotic consumption and usage in humans, 2000–18: a spatial modelling study. The Lancet Planetary Health. Elsevier BV.