A heart attack or angina is a case of referred pain, where pain is sensed at a location other than the site of injury. This happens due to a mix-up of pain signals in the brain.
We have all seen characters in movies experiencing a heart attack or angina, and they often initially experience it as pain in the left arm or the left side of their chest. Have you ever thought about why a problem in someone’s heart would cause pain in their arm instead? Why doesn’t the same thing happen when you have a headache?

We never hear someone say that a sudden pain in their right leg is actually because of their migraine, so why does this happen in some cases and not others? Let’s find out!
Recommended Video for you:
The Mechanism Of Pain Perception
Pain is simply a feeling that originates from an external stimulus that is harmful to us. We can perceive pain because the tissues, muscles, and joints in our body have the endings of certain sensory neurons embedded within them.
While the “tail” or ending rests in different parts of our body, the “head” of neurons lies collected together in clusters embedded in our spinal cord. At each portion of our lengthy spinal cord lies information collected from such “tails” that end in different tissues near that level.
For example, one part of the spinal cord will collect information from various upper portions of the body, such as the chest, arms and nearby internal organs.
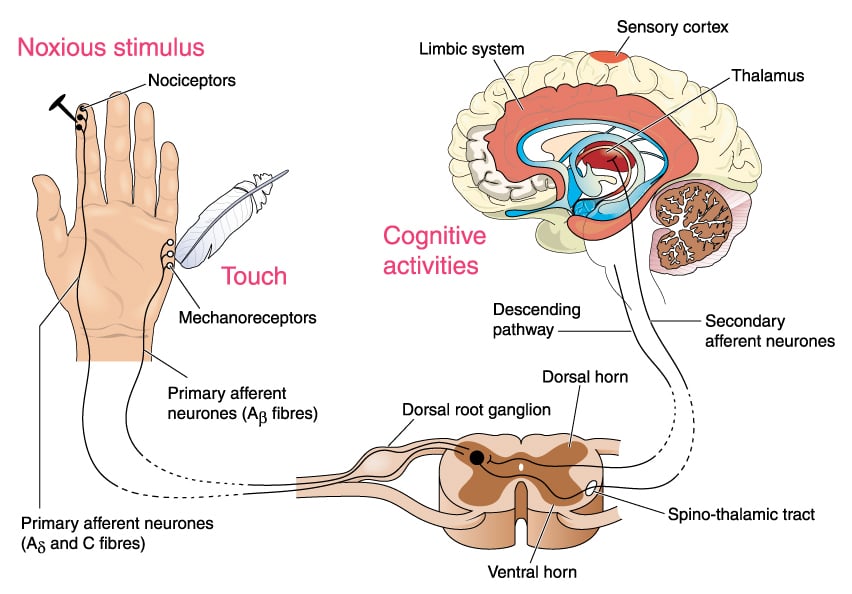
These nerve endings serve as ‘receptors’ that detect external harmful stimuli of mechanical, thermal, or chemical origin and are termed “nociceptors”. A hammer hitting your hand is a mechanical stimulus, but the flame from a candle near your hand is a thermal stimulus.
In this way, our body can detect a variety of harmful stimuli that it comes into contact with externally. Our visceral organs are also innervated by these nociceptors, which detect harmful mechanical, thermal, and chemical stimuli that occur internally.
Once the stimulus causing the pain reaches the nociceptors, they send that information towards a specific portion of the spinal cord. From here, information travels upwards to our brain, which results in us consciously perceiving that pain.
Referred Pain – A Curious Case Of A Signal Mix-up
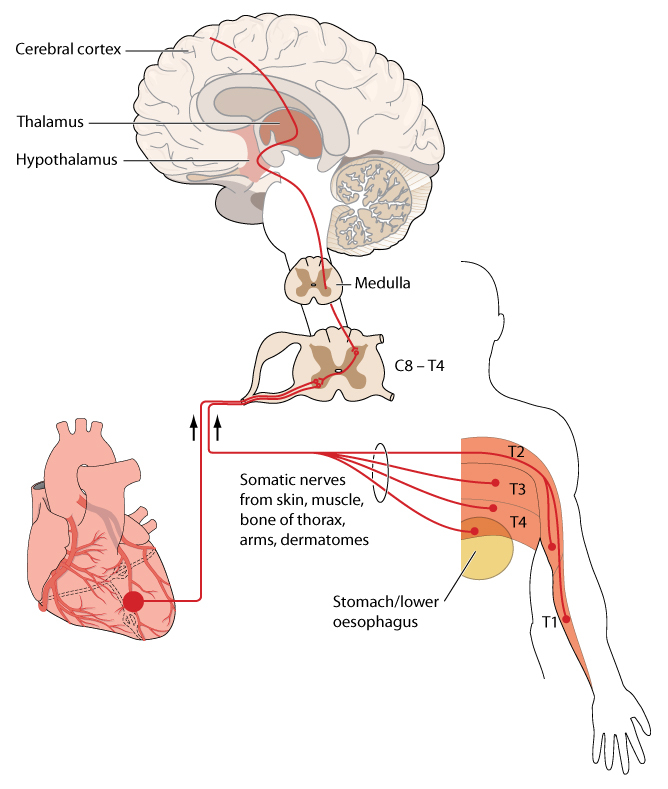
After reading that, the mechanism by which our body senses pain seems too highly organized and methodological to let any error occur. However, this same organization and mechanism is the reason why angina of the heart is felt in the left arm. This curious phenomenon, where pain coming from a visceral organ, such as the heart, is mistakenly perceived as originating from other external body parts, such as an arm, is called “referred pain”.
Let’s recall how information from nociceptors in body parts located next to each other are carried to the same portion of the spinal cord. Let’s say nociceptor A innervates the heart, while a different nociceptor B innervates the nearby left arm, and another one called nociceptor C innervates the left side of the chest. A, B, and C all collect information and converge onto a single higher-order neuron D in the spinal cord.
Now, when D carries information from the spinal cord to our brain, it only receives an input informing us that pain is coming from D, but it is not able to distinguish between A, B, or C.
Therefore, our brain is unable to tell the difference between pain in the internal organ and the skin nearby. If we take the example of an angina, the brain can’t tell if the pain is coming from the heart or the left arm or chest, as the same neuron handles all of these and reports accordingly to the brain.
Thus, we can say that referred pain results from a genuine mix-up of pain signals in our brain as it interprets the incoming information from our body!
Is Referred Pain Unique To Angina Or A Heart Attack?
Referred pain is most familiar to people in the form of a heart attack, but this phenomenon also occurs in other internal organs of the body. An injury in the spleen or stomach can be perceived as pain in the shoulder blade or upper back. Similarly, an injury in the kidney, colon or spinal cord is felt as though it is stemming from the lower back or lower limbs of the body.
Curiously, there are also cases where the reverse occurs – pain in the body is sensed as if coming from an internal organ. The ‘brain freeze’ felt when we hurriedly eat our favorite ice cream is a prime example of this. In this case, we sense the pain as if it is coming from our brain, whereas the actual origin site of the pain is our mouth!

Unfortunately, having conscious knowledge of the phenomenon of referred pain cannot alter our perception of it. This is because referred pain stems from information at the level of the spinal cord, of which we are not conscious. Only when this information arrives at the brain do we become consciously aware of it.
Conclusion
Referred pain is a strange phenomenon where we sense pain in one part of our body, even though the original site of injury is somewhere else. This is a very common phenomenon that can underlie both a serious medical issue, such as a heart attack, as well as a harmless ‘brain freeze’.
Understanding the mechanism of referred pain has several implications in medical science, namely to identify serious ailments from seemingly disconnected symptoms that we experience.
The phenomenon of referred pain is a genuine example of a signal mix-up by the human brain. Even the most complex piece of tissue in the world—the human brain—is prone to error. To err is indeed human.
References (click to expand)
- Kandel E. R., Jessell T. M., Schwartz J. H., Siegelbaum S. A.,& Hudspeth A. (2013). Principles of Neural Science, Fifth Edition. McGraw Hill Professional
- Foreman, R. D., Garrett, K. M., & Blair, R. W. (2015, March 16). Mechanisms of Cardiac Pain. Comprehensive Physiology. Wiley.
- Ingle, S. B. (2014). Epithelial cysts of the spleen: A minireview. World Journal of Gastroenterology. Baishideng Publishing Group Inc.
- Bogduk, N. (2009, December). On the definitions and physiology of back pain, referred pain, and radicular pain. Pain. Ovid Technologies (Wolters Kluwer Health).
- Hartel, R. W., & Hartel, A. (2008). Milk Shakes and Brain Freeze. Food Bites. Springer New York.